Osteochondrosis is a widespread disease of the spine that affects the intervertebral discs and cartilage. The cervical and lumbar regions are most susceptible to such processes. Osteochondrosis of the lower back can cause constant pain in the lower back and significantly complicate a person's life. When treating the disease, preference is given to conservative methods, resorting to surgical interventions only in extreme cases.
Causes of lumbar osteochondrosis
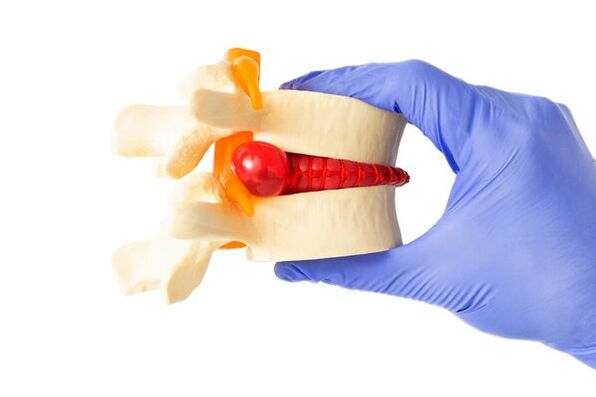
Osteochondrosis is not so much a disease as often a natural phenomenon that occurs as a result of age-related degenerative changes in the spine. Normally, the disc in the lumbar spine acts as a shock absorber between two vertebrae and allows the joints and spine to move easily. The outer part of the disc, the annulus fibrosus, surrounds the soft inner core of the disc, the nucleus pulposus. Everyone's spinal discs undergo degenerative changes as they age, but not everyone develops symptoms.
It is believed that osteochondrosis begins with changes in the fibrous ring, intervertebral disc and subchondral bone. The fibrous ring loses water, which makes it less able to withstand the daily loads on the spine, distributing them incorrectly. Overloading the back of the vertebra leads to arthritis of the joints and hypertrophy (growth, with the formation of osteophytes - bone growths) of the vertebral bodies adjacent to the affected disc.
Reference! According to statistics, 30% of people aged between 30 and 50 have some degree of spinal disc degradation.
There are two main pathophysiological causes of pain in lumbar osteochondrosis. One of the possible causes of pain is inflammation of the nerves as a result of rupture of the outer part of the disc and leakage of the inner core. Inflammatory proteins are released that irritate nervous tissue.
For the second reason, the vertebrae, due to age-related deformation, can no longer effectively absorb the load. This causes abnormal movements of the spine and causes a painful spasm in the back muscles that try to stabilize the spine.
The result of osteochondrosis can be the destruction of segments of the spine, leading to radiculitis. The risk factors that trigger and accelerate degenerative processes in the spine are:
- Hereditary predisposition to diseases of the musculoskeletal system;
- Smoke;
- Previous injuries;
- Hormonal and vascular disorders;
- Excess body weight;
- Muscles that are very weak and do not provide the necessary support to the spine;
- Professional activities associated with heavy physical work (athletes, porters).
Stages of development of lumbar osteochondrosis

Disorders in the intervertebral discs, leading to their degeneration and destruction, occur gradually. The entire pathological process goes through several stages, according to which the stages (or degrees) of lumbar osteochondrosis are distinguished:
- The first stage (degree) is characterized by mild symptoms. Painful sensations develop against the background of irritation of nerve endings by the nucleus pulposus, penetrating into the fissures of the fibrous ring.
- The second stage is characterized by the displacement of the upper vertebra in relation to the lower one, due to cracking of the nucleus and ring. These pathological processes, in addition to pain during movement, cause the occurrence of neurological symptoms, sensations of numbness and instability of the affected area.
- The third phase is characterized by increased pain and the appearance of a herniated intervertebral disc, due to a violation of the integrity of the fibrous ring. Pain, sensory impairment and muscle weakness interfere with daily tasks. Due to compression of the nerve roots, the functioning of the urinary and intestinal systems may be disturbed.
- The fourth stage corresponds to the complete destruction of the intervertebral discs, they become fibrotic and osteochondral growths of the vertebral bodies cause immobility of the spine in this section.
Symptoms of lumbar osteochondrosis
To get started, ask experts for advice:
- Neurologist
- Orthopedist
- Therapist
The main symptom of lumbar and sacral osteochondrosis is pain. It usually worsens when sitting for long periods of time, or when turning, bending the spine or lifting a load. The pain can radiate to the leg, groin and be accompanied by a feeling of numbness and weakness. Moderate, aching, dull pain may be followed by exacerbation attacks.
Symptoms directly depend on the stage of development of the pathology:
- In the initial period, when degenerative changes are just beginning to appear, symptoms are minimal.
- The intermediate stage, characterized by the weakening of the fibrous ring, can now manifest as low back pain.
- In the later phase, when fibrosis develops in the structures and osteophytes form, the pain becomes less pronounced, but the mobility of the spine decreases significantly.
The sensitivity of the lower back may increase when touched. Characteristic sharp pains in the buttocks, thighs and tingling sensation are a sign of compressed nerve roots that occur as a result of degenerative changes in the disc. Patients with lumbar osteochondrosis have difficulty bending forward, backward and to the sides. Osteochondrosis can be complicated by herniated disc and narrowing of the spinal canal, accompanied by the appearance of additional symptoms.
Diagnosis of lumbar osteochondrosis

Diagnosis begins with collecting anamnesis, interviewing and examining the patient. The specialist will be interested in your complaints, physical activity, the presence of old injuries, bad habits and cases of illnesses in close relatives. During a physical exam, your doctor palpates (feels) the lower part of your spine, looking for tender areas, inflammation, or any abnormalities. He may also check sensation and perform motor tests.
The most popular method for diagnosing lumbar osteochondrosis is X-ray examination. The image will show the presence of osteophytes, narrowing of the disc joint space, or the so-called "vacuum" symptom, when gas bubbles are detected in the thickness of the disc. Other methods used are:
- Magnetic resonance imaging showing hydration (degree of saturation with water), shape of the discs, their height, which allows the identification of compressed nerves.
- Computed tomography, which allows you to study the condition of tissues in detail and diagnose disorders in the early stages.
- Provocative discography used to determine the location of the affected disc.
Reference! Magnetic resonance imaging is a very accurate diagnostic method, but it cannot detect rupture of the outer rings of the disc.
Treatment methods for lumbar osteochondrosis
The preferred treatment for lumbar degenerative disc disease associated with chronic pain is conservative treatment with physical therapy, exercise, and medications. For patients with lumbar osteochondrosis it is recommended:
- A daily routine that includes sufficient rest and adequate physical activity;
- Regular physical exercise aimed at strengthening muscles;
- Lifestyle adjustments including nutritional review and weight loss.
Physiotherapy

Several physical therapy techniques have been used successfully to reduce low back pain. Physiotherapy promotes regenerative processes in the disc, stimulates metabolic and transport processes, prevents the formation of adhesions and further damage.
Physiotherapy methods used to treat spinal osteochondrosis include:
- Electrical stimulation. The electrical impulses help to relieve back pain and improve blood circulation in the affected spine.
- Ultrasound therapy. Ultrasound waves can penetrate deep layers of tissue and help relieve inflammation and pain.
- Magnetotherapy. Magnetic fields can improve blood circulation and metabolic processes in tissues, promoting their regeneration.
- Laser therapy. Laser rays can help relieve pain, stimulate blood circulation and stimulate tissue regeneration.
- Ultraphonophoresis. This method combines ultrasound therapy with the use of medications that penetrate deep tissue layers and help relieve inflammation and pain.
Important! Contrary to popular belief, osteochondrosis can and should be treated. Without treatment, it will become a source of chronic pain and can lead to numerous problems, including disruption of the functioning of internal organs.
Drug treatment
To relieve pain that interferes with daily activities, patients are given analgesics and nonsteroidal anti-inflammatories. Depending on indications, the doctor may prescribe stronger medications: muscle relaxants, steroids and narcotic analgesics. Therapeutic blocks are administered with local anesthetics and glucocorticoids to relieve severe pain.
Surgery
Much less often, surgical intervention is used for osteochondrosis of the lumbar region. It may include disc arthroplasty or lumbar spine fusion (creating conditions for the fusion of two vertebrae, while pain is reduced by eliminating movement in this part of the spine).
If spinal movement is significantly impaired, special intervertebral spacers may be installed. For patients who do not respond to all other treatments, a total lumbar disc replacement may be performed.
Treatment of lumbar osteochondrosis at home
The most effective thing you can do at home to maintain functionality and manage pain is to exercise. They will increase the flow of blood, oxygen and nutrients to the spine, helping to keep the cartilage hydrated and the spine flexible for as long as possible. Furthermore, during exercise, endorphins are released, which are natural painkillers.
Frequent position changes also bring relief. Some postures help to deal with a pain attack: kneeling, reclining, lying down. A brief rest is necessary and beneficial, but prolonged bed rest only worsens the condition. It is important to stay active to prevent the disease from progressing. Patients with lumbar osteochondrosis benefit from walking, swimming, cycling, yoga, Pilates, stretching exercises and strengthening the muscle corset. The following measures also help:
- Applying heat to the lower back improves blood circulation and relieves muscle spasms and tension.
- Ice packs help relieve pain and reduce inflammation.
- Massage also relaxes muscles, relieves spasms and reduces pressure on the spine, thus relieving pain. By increasing blood circulation in this area, metabolic processes are improved and tissues are enriched with oxygen.
- Use of orthopedic mattresses and pillows. They will help maintain the correct position of the spine during sleep.
- Correct distribution of the load on the column. When lifting heavy objects, you must use proper lifting technique to avoid straining your lumbar spine.
- Proper nutrition. Eating a balanced diet rich in calcium and vitamins will help maintain healthy bones and joints.
However, if you experience pain or other symptoms, before starting osteochondrosis treatment at home, you should consult your doctor to receive more accurate recommendations and assess the condition of your spine.
Which doctor should I contact for lumbar osteochondrosis?
If symptoms characteristic of lumbar osteochondrosis appear, it is recommended to consult a neurologist or orthopedist. If you have lower back pain, you can also make an appointment with a therapist. He will prescribe the necessary tests to make the diagnosis and refer you to a specialist.
Treatment of lumbar osteochondrosis
Specialists from the nearest clinic in your city or other location are ready to understand the reasons and help you deal with the pain. Doctors usually have extensive clinical experience and have mastered all modern methods of treating and diagnosing osteochondrosis in women and men. For the most part, convenient location, excellent equipment and versatility of institutions are priorities of modern medicine, which allow you to quickly carry out any examination and restore the health of the musculoskeletal system. You can make an appointment by calling the clinic that is most convenient for you, as well as on the website by filling out the online form.
Prevention of lumbar osteochondrosis

Effective methods for preventing lumbar osteochondrosis are:
- Regular physical activity. Stay in good physical shape. Strengthen your back muscles. Stretching and strengthening exercises for the back help keep the spine healthy.
- Reduce stress on the spine: Avoid unnecessary stress on the spine. When lifting heavy objects, use proper lifting techniques.
- Posture correction: ensure correct posture. Sit and stand, don't relax. Choose an orthopedic pillow and mattress for sleeping in order to maintain the correct position of the spine during rest. Buy quality shoes with good cushioning and support.
- Take care of your back support by using orthopedic chairs if, due to the nature of your profession, you are forced to sit for long periods of time. Avoid staying in the same position for a long time. Take regular breaks and stretch your spine.
- Watch your weight. Excess weight can cause additional stress on the spine.
- Avoid uncontrolled movements and back injuries. Be careful when playing sports or physical activities.
- Quit smoking, which can negatively affect spinal health.
By following simple recommendations, you can live an active and fulfilling life, minimizing the risk of back pain. If you already have symptoms, pain in the lumbar spine, consult a doctor for diagnosis and treatment.
























